Fentanyl Addiction Treatment and Rehab
Fentanyl: A Potent Synthetic Opioid
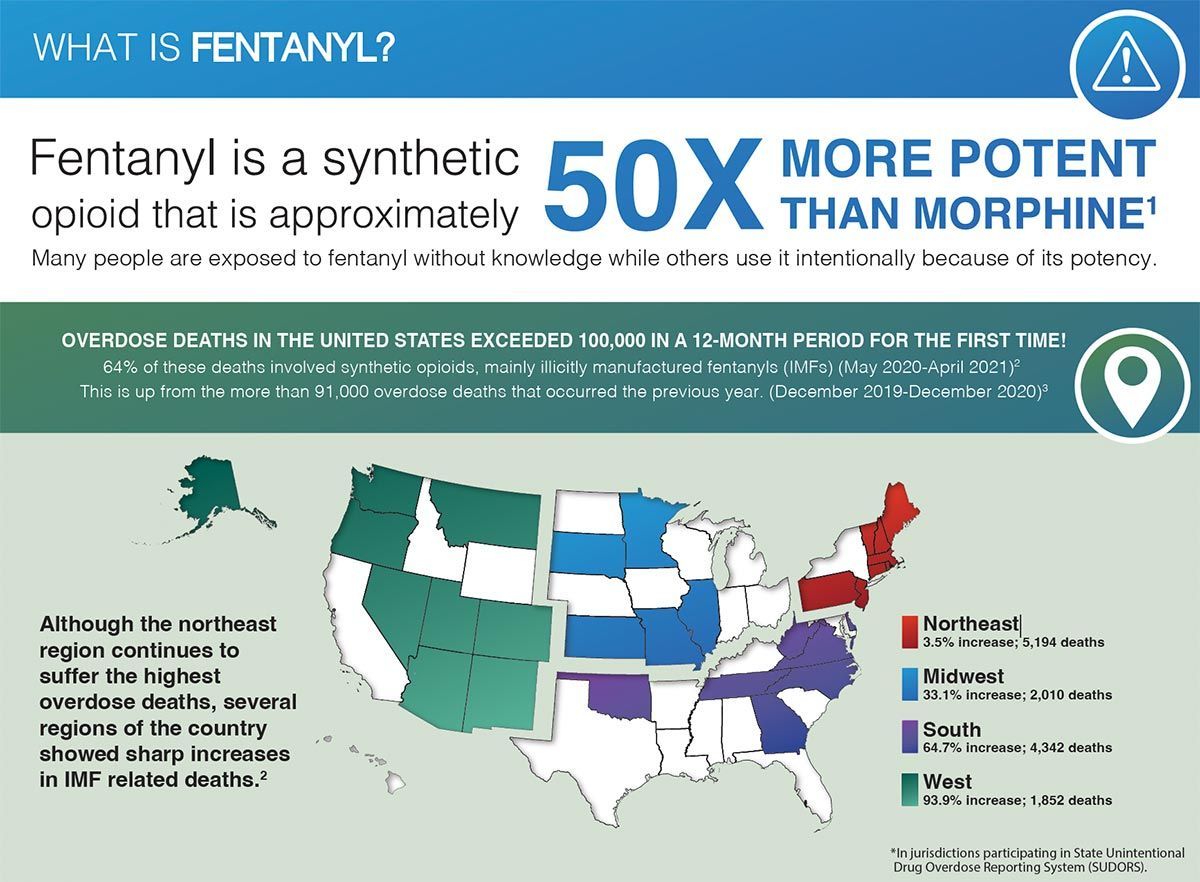
Fentanyl is a synthetic opioid known for its potency—50 to 100 times stronger than morphine. While often used in hospitals after major surgeries, it can also be misused. Illegal production poses serious risks for users.
Prescription fentanyl is also known as:
- Sublimaze
- Duragesic
- Actiq
Street names for fentanyl include:
- Dance Fever
- Goodfellas
- Murder 8
- Tango & Cash
- Jackpot
- Friend
- Apache
Complete the pre-screen form below to initiate the admission process. Our admissions team will contact you shortly.
What Makes Fentanyl So Dangerous?
Fentanyl poses a significant risk due to its extraordinary potency compared to other opioids, urging healthcare professionals and the public to recognize its dangers. As a synthetic opioid, it is 50 to 100 times stronger than morphine. Even a tiny amount can have intense, dangerous effects, increasing the risks for those who encounter it. Consequently, fentanyl requires strict controls and precise administration, as the margin for error is minimal and can lead to fatal outcomes. In 2017, reports indicated fentanyl was linked to over 50% of opioid-related deaths in the U.S., highlighting the critical public health crisis it presents and the need for effective educational campaigns to prevent misuse and promote safety.
How Do People Use Fentanyl?
Prescription fentanyl is available as a shot, lozenge, or patch. Lozenges release medication gradually when sucked, while patches allow slow absorption through the skin for prolonged effects. Injections, administered by anesthesiologists, provide immediate results.
Illicit fentanyl comes as eye drops, nasal sprays, pills, powder, or on blotter paper. It is often mixed with heroin, cocaine, MDMA, or methamphetamine to enhance effects. However, its potency can lead to overdose, as even a small excess poses serious risks.
What Are the Symptoms of Fentanyl Abuse?
The use of fentanyl can lead to a variety of symptoms. Some of the side effects associated with fentanyl include:
- Intense short-term highs
- Euphoria
- Nausea
- Fainting
- Seizures
- Fatalities
- Slowed breathing
- Lowered blood pressure
- Constricted pupils
- Sedation
- Vomiting
- Urinary retention
Depending on the dosage, fentanyl can cause sedation, lowered blood pressure, slowed respiration, or seizures, potentially leading to coma or death.
Is Fentanyl Dangerous?
Fentanyl poses a significant danger because it is easy to overdose on. An overdose happens when a person takes more fentanyl than their body can handle, leading to hypoxia, where the brain lacks oxygen. Without prompt treatment, this can result in death.
What Are the Methods of Fentanyl Abuse?
When misused, fentanyl is often injected, snorted, taken as a pill, or applied to blotter paper. Individuals with prescription gel patches may misuse them by extracting the gel for ingestion or injection. The DEA has noted cases of patches being cut and placed in the cheek or under the tongue. Illicit fentanyl may also be mixed with substances like heroin, cocaine, MDMA, or methamphetamine, greatly increasing the risk of severe side effects and overdoses.
Identifying Signs of a Fentanyl Overdose: What to Look For
A fentanyl overdose presents several clear symptoms. Among the most prevalent signs of an overdose are:
- Unconsciousness.
- Alterations in pupil size
- Respiratory failure
- Cyanosis
- Cold, clammy skin
- Coma
Respiratory depression, coma, and pinpoint pupils indicate opioid poisoning. If you see these symptoms, seek emergency medical help immediately. Failing to act can lead to serious injury or death.
What Are the Treatments for a Fentanyl Overdose?
A fentanyl overdose can be quickly treated with Naloxone, an opioid antagonist that reverses opioid effects. Commonly known as NARCAN, it is available to EMS, law enforcement, pharmacists, and other authorized personnel. Many individuals prescribed opioids also receive NARCAN to ensure access during accidental overdoses.
What Symptoms Indicate Fentanyl Withdrawal?
Like other opioids, fentanyl has unique withdrawal symptoms to note. Possible symptoms include:
- Muscle aches
- Restlessness
- Lacrimation
- Anxiety
- Frequent yawning
- Difficulty sleeping
- Runny nose
- Excessive sweating
- Goosebumps on the skin
- Rapid heart rate
- High blood pressure
- Dilated pupils
- Nausea
- Vomiting
- Abdominal cramping.
How Long Does Fentanyl Withdrawal Last?
Withdrawal symptoms are usually short-lived. For most, they start to improve within 72 hours and diminish significantly within a week.
How Are Symptoms of Fentanyl Withdrawal Treated?
Fentanyl withdrawal symptoms can be very distressing and carry significant risks. This underscores the importance of seeking medical treatment in a regulated setting, as patients often achieve better outcomes than those who try to quit or reduce dosage on their own. During detox, it's essential to recognize the varying degrees of withdrawal, which can range from mild to severe, and complications may also arise.
Mild Withdrawal
Mild withdrawal from fentanyl can be uncomfortable but is usually not life-threatening. It can often be managed with over-the-counter medications like ibuprofen or acetaminophen. Staying hydrated and getting enough rest helps, while hydroxyzine and loperamide can alleviate nausea or diarrhea.
Intense Withdrawal
When patients have severe symptoms, hospitalization may be needed during withdrawal and detox. Clonidine can reduce symptoms by 50 to 75%. Other medications include Suboxone (naloxone and buprenorphine) and methadone, which aid in managing withdrawal by lessening severity and duration. Methadone, while an opioid for long-term maintenance, is safer due to its controlled use compared to stronger opioids.
Complications of Fentanyl Withdrawal
Opioid withdrawal is typically not life-threatening; however, it can be highly uncomfortable. Patients facing complications may encounter several common issues, including:
- Intense nausea
- Muscle cramping
- Diarrhea
- Vomiting
Given these symptoms, close monitoring is essential. Nausea and vomiting can risk aspiration pneumonia, while diarrhea may cause electrolyte imbalances, leading to circulatory issues or severe complications.
Those with severe muscle cramping may experience significant pain, including acute joint pain. Thankfully, detoxification programs provide options to relieve these symptoms.
What Can You Expect from Monarch Recovery During an Outpatient Rehab Program?
When an individual struggles with fentanyl addiction and seeks help at a detox and rehab facility, the primary objective is to ensure a safe detoxification process. This may involve the use of long-term medications or close monitoring during withdrawal to mitigate severe symptoms, including electrolyte imbalances.
Typically, detoxification begins within six hours of the last drug dose, with symptoms generally fading within up to 10 days. However, withdrawal symptoms are often intermittent, surfacing in waves. The severity usually peaks 72 hours after the final dose before gradually subsiding.
At Monarch Recovery, we focus on facilitating a smooth transition from detox to rehabilitation to provide our patients with thorough care. Once individuals have successfully faced the hurdles of withdrawal, they swiftly progress into our intensive outpatient program. This phase is crucial, as it tackles both the psychological and physical facets of addiction.
Our rehabilitation approach is anchored in dual-diagnosis treatment, designed to identify and address any co-occurring mental health disorders alongside substance abuse. We implement a variety of therapeutic methods, including behavioral therapy, which aids patients in understanding and transforming their thought processes and behaviors pertaining to substance use. Our group therapy sessions cultivate a sense of community and shared experiences, while one-on-one counseling delivers tailored support for personal challenges.
We understand that some individuals may opt not to pursue rehabilitation; however, this choice significantly increases the risk of relapse. Research indicates that, without adequate rehabilitation assistance, the probability of returning to substance use rises dramatically. Thus, we strongly advise that patients engage in both detoxification and rehabilitation within a personalized treatment framework, maximizing their chances of achieving lasting recovery and a healthier future.